Group member Gerhard Sundborn tells NewstalkZB why lockdowns cannot be in place long enough to eliminate the virus. He knocks it out of the park.
By Ananish Chaudhuri and Simon Thornley
The authors are members of the Department of Economics and School of Population Health respectively at the University of Auckland. The views expressed are their own.
During the Vietnam war, the well-known (and Kiwi-born) journalist Peter Arnett is supposed to have quoted a US Major as saying “We had to destroy the village in order to save it.”
Regardless of whether anyone actually said this or not, we cannot help reflecting on the idea behind this as we go into yet another lock-down.
Back in March, when we entered our first lock-down, the evidence was not so clear. Reasonable people could have disagreed about the sagacity of the lock-down. Some of us did but on the whole most were willing to abide by the government’s decision.
But the evidence is clear now. Lock downs are not a panacea. There is, at best, weak if any correlation between lock downs and the spread of the disease. At best, they merely postpone the spread of the infection.
When the Swedish authorities said this, the rest of the world sneered at them.
Now, there is increasing recognition that maybe the Swedes did get it right. Certainly not all of it; they did experience a failure to protect the frail and elderly. But, on balance, it appears they will emerge from the pandemic stronger than their neighbours and that in the current globalized world, lock downs are not and cannot be a sustainable solution.
A recent report from the Productivity Commission now provides support for this Swedish view by asking questions about the relative costs and benefits of prolonging our earlier lock down. The conclusion: the costs conservatively outweighed the benefits of an extended lockdown by 95:1.
And the Swedish approach has been reiterated by Camilla Stoltenberg, Director General of the Norwegian Institute of Public Health; that Norway could have handled the disease without locking down.
There is no vaccine and if there is one, it is still some time away. The fastest vaccine ever developed, for mumps, took four years. In any event, even with a vaccine there is no way of guaranteeing that every Kiwi will take it. In fact, unless we keep our borders closed forever, we need everyone else in the world to take the vaccine too. Diseases we thought had been eliminated, like measles, have made a come-back.
Consequently, in an earlier article we pointed out that elimination is not and never was a realistic strategy and suggested ways of moving forward and resuming normalcy including opening our borders.
It was certainly inevitable that the disease would recur. What was not inevitable was the steps we took along the way and the economic and social costs of those steps.
Did we really need to spend the time, effort and resources to force people into quarantine? Could we not trust them to self-isolate like we did earlier with prosecution of violators? Like Sweden, New Zealand is a high trust society. Why does our government have such little faith in its citizens? Why does it claim for its police the right to enter people’s home without warrants to enforce quarantine?
And if a government does not trust its citizens, then why and how long should the citizens continue to trust the government?
Even with preponderance of evidence that lock downs are mostly useless, our government has responded to an outbreak with another lock down. The initial rationale for a lockdown was protecting our hospitals, but now with cases linked to only one household, the threshold for pulling the lockdown trigger has dropped considerably.
Is this really sustainable: To lurch from one from lock down to another with breaks in between?
Yes, resuming normal life will lead to more cases and there will be more deaths due to Covid-19; just as there will be more deaths from auto accidents, flu, pneumonia, respiratory illnesses, loneliness and self-harm. We also now appreciate that the age distribution of deaths from Covid-19 is indistinguishable from background mortality.
Maybe we need to better confront the idea of our own mortality. Such a conversation is topical given the upcoming referendum on euthanasia.
If we could shut down all motorized vehicles, then the reduction in pollution will save many lives that are lost from respiratory illnesses. But, no one suggests that since this is not a realistic proposition. Instead, we set emissions standards in such a way that the social benefit of driving or flying is equal to or higher than the social cost.
Contrary to the culture of fear besetting us, Covid-19 is hardly the threat it has been made out to be. Both the case fatality ratio (number of deaths divided by the number of reported cases) and the infection fatality ratio (number of deaths divided by the number of people potentially infected) is relatively low and much lower than say Ebola or other corona viruses such as Middle Eastern Respiratory Syndrome (MERS) or Severe Acute Respiratory Syndrome (SARS). It is now clear that lockdowns are a blunt instrument that is disproportionate to the threat posed by this virus.
Media Release
14 August 2020
Epidemiologist Simon Thornley has reassured people that there has been no new information that concludes masks are warranted against COVID19.
“The trials are clear; there is no statistically useful safety gain in wearing a mask, although low quality observational studies show an advantage to wearing one in confined spaces.”
Thornley says he was moved to clarify the science because people advocating masks were claiming ‘things had changed’, leading to an increase in public mask-wearing since Wednesday.
“Nothing in medical science has changed since Ashley Bloomfield first told us months ago that there was no advantage to masks. What has changed is social and political advantage in advocating masks, and that’s not science.
“I will not be wearing a mask without symptoms, but anyone with compromised health could choose to carry a mask to wear in places like public transport.”
Thornley urged all public communicators, including media, to reference the latest science on masks so people could decide for themselves (see below).
On Monday, the Covid Plan B group is live streaming a COVID-19 Science and Policy Symposium, featuring international experts analysing the New Zealand situation. Find out more here.
ENDS
The Science on masks
A trial in Australia showed that in households exposed to children with respiratory symptoms and fever, there was no difference in outcome between households that wore either surgical or P2 masks with controls who did not wear masks. The incidence of laboratory confirmed infections were twice as high in the mask wearing groups compared to controls, but the difference was not statistically significant.1 About 50% of patients reported problems with the masks, and by day five, only 30% of participants were compliant with the mask use.
A larger trial in Thailand that compared control, to handwashing, and handwashing and surgical masks in households with influenza-like illness showed no difference between the three groups, in terms of reducing the incidence of secondary transmission from primary cases.2
Meta-analyses of observational studies have reported benefits of reductions in risk of using masks.3 A case-control study of H1N1 transmission following a prolonged flight between China and the US showed a very strong association between mask use and protection from infection. None of the 9 cases wore masks, compared to 47% (15/32) of control passengers.4
The World Health Organisation5 only recommends masks when individuals have symptoms compatible with Covid-19. In populations such as those with a high prevalence of Covid, immunocompromised patients or times where high population density cannot be avoided, such as mass gatherings, public transportation (including aeroplanes), masks are considered useful for ‘source control’, rather than ‘protection’.
References
- MacIntyre CR, Cauchemez S, Dwyer DE, et al. Face mask use and control of respiratory virus transmission in households. Emerging infectious diseases 2009;15(2):233.
- Simmerman JM, Suntarattiwong P, Levy J, et al. Findings from a household randomized controlled trial of hand washing and face masks to reduce influenza transmission in Bangkok, Thailand. Influenza and other respiratory viruses 2011;5(4):256-67.
- Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. The Lancet 2020;395(10242):1973-87. doi: https://doi.org/10.1016/S0140-6736(20)31142-9
- Zhang L, Peng Z, Ou J, et al. Protection by face masks against influenza A(H1N1)pdm09 virus on trans-Pacific passenger aircraft, 2009. Emerging infectious diseases 2013;19(9):1403-10. doi: 10.3201/eid1909.121765
- Organization WH. Advice on the use of masks in the context of COVID-19: interim guidance, 5 June 2020: World Health Organization, 2020.
Media Release
13 August 2020
Epidemiologist Simon Thornley says the new virus outbreaks and lockdown responses are proof that New Zealand must, as the WHO has recently said, learn to live with the virus.
“An outbreak was inevitable, and therefore lockdowns were never a viable repeatable solution – you pay a high price, repeatedly.”
“As we’re about to experience yet again, lockdowns harm everyone more than the coronavirus does.”
“Protecting the elderly, staying at home if you are ill and hand hygiene are the mainstays of reducing the spread of the virus.”
Thornley says it is ironic that the Government had now also decided to lock down all aged care facilities.
“This is precisely the solution we advocated three months ago. Proof has since mounted that those of us over 65 are the only people at real risk: the age of death with this virus is much the same as what we observed in people who died last year. The risk is extremely low for people aged less than 65. No one has yet died in their fifties or younger in New Zealand.
Even in apparently ‘hard hit’ regions of the world, people aged less than 65 without underlying conditions were very unlikely to die from the virus. They accounted for 0.7–3.6% of all COVID deaths in France, Italy, Netherlands, Sweden, Georgia, and New York City.
“Safe hygiene practices and protection of the elderly is the best solution.” Thornley said.
Thornley points out that the Government promised that the first lockdown was to eliminate the virus, and its four-day extension would ‘lock in the gains’.
“Yet here we are, with the virus, locking down again. Proof, if you needed it, that lockdowns only delay, or even magnify, the health and economic harm.”
On Monday 17 August, the Covid Plan B group is live streaming the COVID-19 Science and Policy Symposium, featuring international experts analysing the New Zealand situation.
The international speakers confirmed include founder of Yale University’s Yale-Griffin Prevention Research Centre Dr David Katz, who worked at the front line of New York hospitals dealing with patients, and viral immunologist Dr Byram Bridle who is part of a team commissioned by the Canadian Government to develop a COVID vaccine.
To find out more information about the COVID-19 Science and Policy Symposium, visit here.
ENDS
“If safe and effective vaccines and life-saving preventative and therapeutic medications are not found, lengthy lockdowns prove impossible, and the pandemic does not disappear spontaneously, population immunity is the only, long-term solution.
“I am not advocating that we dispense with all control measures, we still need to wash our hands, keep our distance and do everything we are being advised to.
“The bottom line is that older people have got a lot to gain from lockdowns and a lot to lose from the infection. Young people have a lot to lose from lockdowns and not much to lose from the infection.”
Raj Bhopal, emeritus professor of public health at Edinburgh University.
https://www.nzherald.co.nz/world/news/article.cfm?c_id=2&objectid=12352932
Media Release
28 July 2020
Several World Health Organisation officials have this week crystallised New Zealand’s border dilemma – saying that keeping national borders closed because of COVID-19 is now unfeasible.
Head of WHO’s emergencies program lead Mike Ryan said “it is going to be almost impossible for individual countries to keep their borders shut for the foreseeable future…. Economies have to open up, people have to work, trade has to resume.”
Simon Thornley, of the Covid Plan B Group, says this highlights a core problem the group had with lockdown; there was no exit strategy.
“New Zealand came out of lockdown well, but the suppression strategy has left us in an international and economic dead end.
“Other nations, although worse hit by cases and deaths, are now opening up borders and activity. New Zealand is in a bind; locked behind its border, fearful of even a single infection let alone a death.
“Yet the most recent infection fatality studies show Covid-19 is 0.65% – at most only a quarter of the deaths we expected, and probably far fewer.
“We need to open our borders to restore economic and social connections with the rest of the world.”
Thornley said New Zealand’s dilemma would be tackled by an international symposium at Parliament on 17 August, featuring several internationally respected experts. They will analyse the latest information on COVID-19 to offer possible pathways for New Zealand’s recovery.
“The main danger of the virus is that hospitals become overwhelmed and the virus spreads to frail patients. Most countries are now well beyond this, but New Zealand might not be. We need to cautiously open our borders and continue to monitor our health system’s capacity.”
The international speakers will present live by video link, followed by questions from the public. They include vaccine specialist Byram Bridle, Epidemiology Professor Sunetra Gupta of Oxford University, and Preventative Medicine specialist David Katz at Yale.
Interested parties can register for free tickets here. To find out more information about presenters at this event, please visit here.
ENDS
Simon Thornley
27/07/2020
Most New Zealanders believe now that we are in an exalted position on the Covid road. We are world leaders who have beaten a deadly virus thanks to a tough lockdown. Our only threat now remains from overseas travelers who are quarantined at the border. We are now a Covid-19 free paradise. We can stay this way until a promising vaccine from Oxford comes our way. Surely, this is a matter of holding on for a few more months, and then we can put this whole episode behind us and get on with life.
I would like to believe this story, since my life would be much simpler if I followed the official line. But as an epidemiologist, I’m taught to question and to examine the evidence independently. There are a number of assumptions in this story we have been told. Let’s examine them one by one.
The first is that we are dealing with a deadly virus. Early on in the pandemic, it was possible to believe this, as we had only genetic tests of the virus available. The ratio of people who had died with Covid-19 divided by people who tested positive was 3.4%. This is about seven times the usual estimates of fatality from seasonal influenza (<0.5%).
High fatality rates were projected on a grand scale by modelers. These high rates lead to astronomical predictions of death and destruction which justified severe lockdowns.
Throwing the kitchen sink at such a deadly threat made sense. Just as with swine flu in 2009, however, it was soon found that other evidence, such as antibodies detected in blood, showed a totally different pattern. This occurred in 2009 when antibodies were discovered in about one in four of the New Zealand population. The clamour to eliminate the virus lost its legs.
Early in the epidemic, other researchers overseas were pointing to similar evidence. Professor Mikko Paunio, for example, an epidemiologist from Finland, early in the epidemic showed that 27/1000 blood donors had antibodies to the virus in Copenhagen, Denmark. This proportion extrapolated to over a million Danes having seen and recovered from the virus, compared to many fewer ‘official’ cases. The revised fatality rate was 0.13% – nothing to get excited over.
Now, we even have the Center of Disease Control in the US using 0.65% as a working estimate. This is derived from a summary paper which averaged the results of 26 individual studies. This revised figure is in the scale of severe influenza, and scales down the threat of the virus to just above that of seasonal influenza. These estimates don’t take into account more information about T-cells which now show an even wider exposure to the virus than from antibodies alone. This means that even these revised estimates are very conservative and should be lower still.
In New Zealand, it is clear from looking only at cases, that risk of fatality is higher for older people (Table). People aged over 90 years have not fared well after infection, but conversely, we have now had no deaths from the virus in people aged under 59 years.
Table. Covid-19 cases in New Zealand, by clinical status and age group (at 20 July 2020).
| Age Group (years) | Active | Recovered | Deceased | Case fatality ratio* (%) | Total |
| 0 to 9 | 1 | 37 | 0 | 0 | 38 |
| 10 to 19 | 0 | 122 | 0 | 0 | 122 |
| 20 to 29 | 8 | 365 | 0 | 0 | 373 |
| 30 to 39 | 9 | 239 | 0 | 0 | 248 |
| 40 to 49 | 1 | 221 | 0 | 0 | 222 |
| 50 to 59 | 3 | 247 | 0 | 0 | 250 |
| 60 to 69 | 2 | 177 | 3 | 1.67 | 182 |
| 70 to 79 | 2 | 71 | 7 | 8.97 | 80 |
| 80 to 89 | 0 | 23 | 7 | 23.3 | 30 |
| 90 or more | 0 | 4 | 5 | 55.6 | 9 |
| Total | 26 | 1506 | 22 | 1.44 | 1554 |
*The ratio of deceased PCR test-positive cases divided by the sum of both deceased and recovered. The infection fatality ratio is likely to be much lower owing to serology and T-cells pointing to more widespread infection compared to PCR test-positive cases only. 95% confidence intervals calculated by exact binomial method. CI: confidence interval.
Source: https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-current-situation/covid-19-current-cases Accessed 20 July 2020.
It is also clear that around the world the average age of death of Covid-19 patients is near that of the average life expectancy of that country. This is also clear for New Zealand (figure 1), where the shape of the age distribution of Covid-19 deaths closely approximates the spread of deaths over the same period the year before. A formal test for differences in counts between these data sources shows no evidence of difference. It is very difficult to argue from this plot, that Covid-19 is shortening life spans.
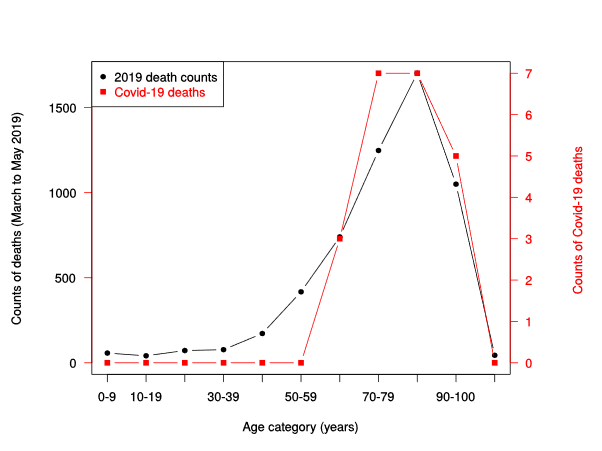
Figure 1. Counts of NZ deaths March to May 2019 (black line), compared to counts of deaths from Covid-19 (red line, right vertical axis), by age category.
Sources: https://fyi.org.nz/request/12583-number-of-deaths-by-age-group-and-week-for-the-last-5-years-dia
https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-current-situation/covid-19-current-cases Accessed 20 July 2020.
Although commentators are lampooning Sweden and their Covid-19 death rates, it is clear that countries with harsh lockdowns, such as Peru have higher rates of Covid-19 deaths than Sweden. Belgium, UK and Spain, all locked down but suffered higher rates of Covid-19 deaths than the comparatively liberal Swedes. Just what explains the difference between these country’s rates of Covid deaths is still unclear, but much is likely to be explained by differences in recording of deaths, demographic differences and population density. We now know that national lockdowns during the epidemic are not associated with an expected reduction in Covid-19 deaths.
Despite the avalanche of evidence coming from overseas, the New Zealand Ministry of Health has clearly stated that it has little interest in serology and is not planning a serosurvey. This strongly indicates that an updating of the fatality of the virus is unlikely in New Zealand, at least in official circles.
Where does this leave New Zealand? Our borders remain closed and both political parties are doubling down on this action. In contrast, other countries including the vast majority of Europe, Iceland, China, and the UK are opening up their borders. Iceland has had its borders largely opened, albeit with virus screening, since June 15 with no evidence of a further outbreak (figure 2). It is clear that these governments have learned from new information, reassessed the risk posed by the virus to their populations, including their immune status.
Evidence of widespread immunity, both in the form of antibodies and T cells is growing. In New Zealand, our politicians and health leaders have little interest in investigating this important issue. A vaccine is simply not a realistic proposition for at least another four years, if not ten. Our tourist economy and borders simply cannot wait this long. We will be held hostage to a story associated with the virus that is well past its “used by” date.
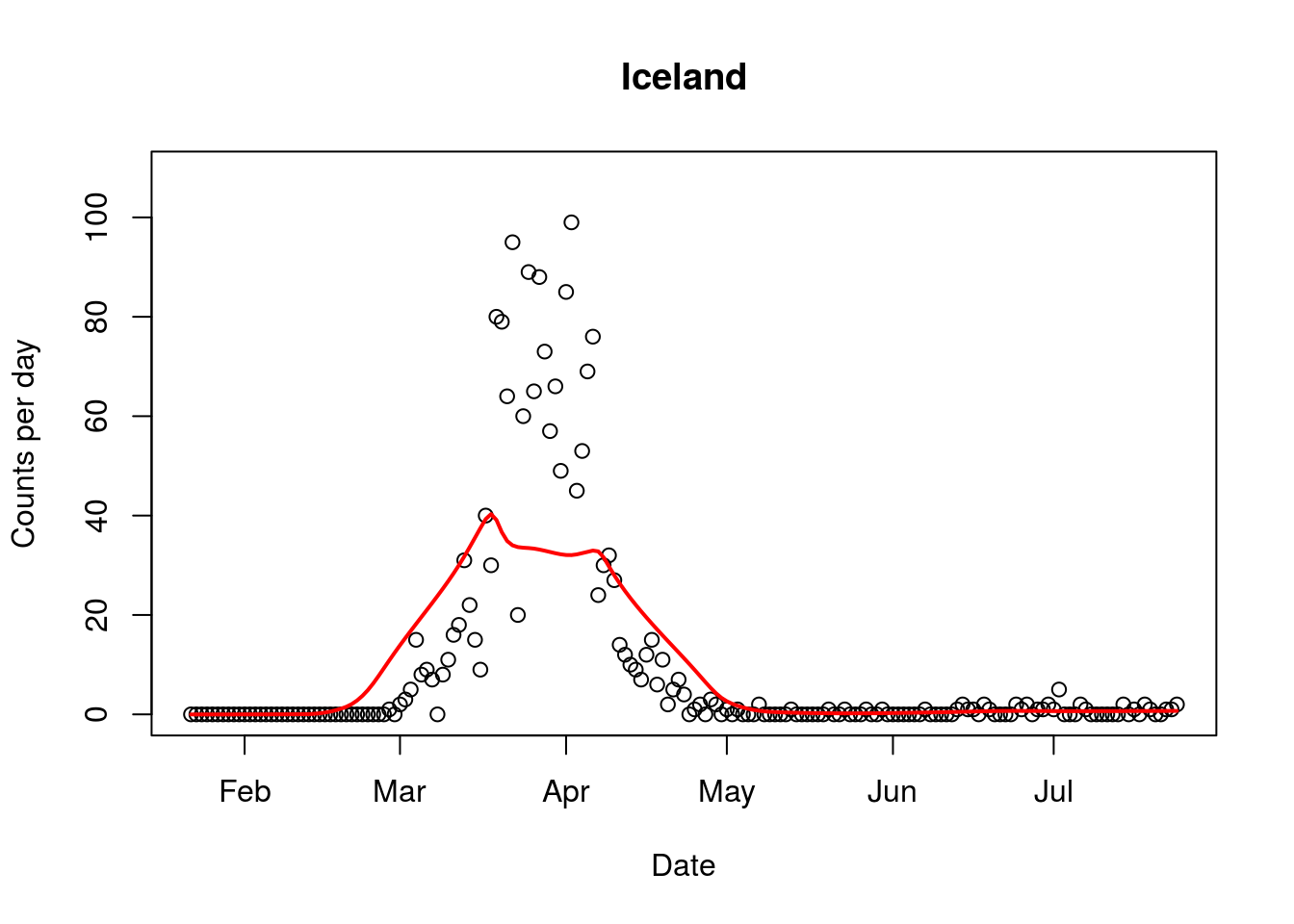
Figure 2. Covid-19 epidemic curve from Iceland, with border opening occurring in mid June. Red line indicates average trend.
Media Release
21 July 2020
An Oxford professor has criticised New Zealand’s Covid-19 strategy ahead of an international symposium on New Zealand’s policy options to be held in Parliament in August.
Professor Carl Heneghan from the Oxford Centre for Evidence Based Medicine said in an interview on the weekend that “If you follow the New Zealand policy of suppressing it to zero and locking down the country forever, then you’re going to have a problem… This virus is so out there now, I cannot see a strategy that makes suppression the viable option. The strategy right now should be how we learn to live with this virus”
Simon Thornley, of the Covid Plan B Group, has today announced plans to hold an international symposium on New Zealand’s policy options at Parliament on 17 August.
The COVID-19 Science and Policy Symposium will feature at least five internationally respected academics and scientists analysing the latest information of COVID-19 to offer possible pathways for New Zealand’s recovery, along with New Zealand-based experts.
Thornley says experts were keen to present at the symposium because New Zealand is receiving global attention for its handling of the pandemic and the situation it is now in.
“New Zealand’s approach is a hot topic internationally – experts are keen to discuss our unique position. Our low infection and death rate has created a difficult decision on when and how we open back up to the world.
“The risks and impacts of the virus are now becoming much clearer and more certain. This information is vital to New Zealand’s decision-making, but we’re not getting the full picture.”
The international speakers will join by video link, giving presentations on the latest data, and open to discussion and questions from the public.
Those confirmed include Dr David Katz, founder of the Yale-Griffin Prevention Research Centre and who worked at the front line of New York hospitals dealing with patients, and viral immunologist Dr Byram Bridle who is part of a team commissioned by the Canadian Government to develop a vaccine.
The COVID-19 Science and Policy Symposium will be held in Parliament’s Banquet Hall on Monday 17 August. Interested parties can register for free tickets here.
To find out more information about presenters at this event, please visit here.
ENDS
In a stunning interview, Professor Carl Heneghan from the Centre for Evidence Based Medicine at Oxford says:
“If you follow the New Zealand policy of suppressing it to zero and locking down the country forever, then you’re going to have a problem… This virus is so out there now, I cannot see a strategy that makes suppression the viable option. The strategy right now should be how we learn to live with this virus.
“The benefits of the current strategy are outweighed by the harms…When it comes to suppression, only the virus will have a determination in that.”
https://unherd.com/thepost/oxford-epidemiologists-suppression-strategy-is-not-viable/
Media Statement
8 July 2020
The Government has formally confirmed that it will not use any of the current or future serology tests to assess how widespread the Covid19 disease has been in New Zealand.
In answer to an Official Information Request by the Covid Plan B group, the Director of the COVID-19 Health System Response team in the Ministry of Health said serology tests would underestimate the true level of exposure to Covid-19.
Epidemiologist Simon Thornley says the new policy is the opposite of what was done in 2009 when serology data on low prevalence of swine flu convinced health officials not to take extreme control measures.
“Serology testing will underestimate the true prevalence, but that will be many times more accurate than just guessing from tests of people presenting with symptoms.
“Fear and uncertainty are driven by lack of information. The more we know, the better we can fight disease. It has been the policy in the past, so it’s strange not to do it now.”
Thornley says a consistent picture is emerging that nose tests for Covid-19 are only picking up a small fraction of all cases.
“Antibodies, present in the blood as well as T cell immune responses to the virus are revealing the coronavirus has reached far more people than listed in the daily “cases” statistic.
“That is important because it would reveal the true effectiveness of our protective measures, and the true state of our population immunity to coronavirus.”
In response to the OIA request for data from serology testing, the Government confirmed:
“Currently there are no Ministry sanctioned seroprevalence studies being performed”.
It claimed that this was supported by a letter in the Nature Medicine journal which indicated that one study found variability in individuals; 40% of asymptomatic people became seronegative and 13% of symptomatic people became negative for IgG [An immunoglobulin] as they recovered.
It noted that a study had been undertaken by the Southern DHB, and that “Positive COVID-19 cases from the Southern DHB study will be confirmed on a second assay to increase positive prediction value.” It said “future studies will have to learn from the Southern DHB study and adapt its methodology accordingly.” The Ministry added that there had been blood mononuclear cell collection by the University of Otago which would be used to perform future mediated response testing.
/ends
Contact Simon Thornley 021 299 1752
