17 November 2020
Byram Bridle, a viral immunologist at the University of Guelph, cautions New Zealanders that the lead vaccines against Covid19 may not be the solution they are expecting to end its isolation under the elimination strategy.
The main points of his caution are:
- NZ will have to wait at least two years before the Pfizer vaccine is available, because it is in strict isolation and low on the priority list for the 500m doses available in 2021.
- Not enough data has been released to know whether the vaccine prevents or weakens the symptoms of Covid19, or how long the protection will last.
- The safety data will be incomplete if it is approved for use next year, so monitoring will need to be carried out on vaccinated people for some years.
- The Pfizer data has not been rigorously peer-reviewed.
- There is no available data on the qualitative nature of the immune response. Vaccines like this can be misinterpreted by the immune system as an extracellular pathogen, which can cause them to respond poorly to natural infections with future coronaviruses.
“Pfizer’s vaccine is a RNA-vectored vaccine. This technology is relatively new and has not been approved for clinical use before. The company has been able to move surprisingly fast. If the recent data is indicative of what data from the rest of the trial will look like, there is a good chance the vaccine could receive emergency approval by early in 2021.
However, there are many nuances…”
Insufficient public data
“The study is only partially complete. There exists the possibility that the final data set will fail to secure regulatory approval (but it looks like they may be on track).
Data that accompanied the Pfizer press release was extremely superficial and, therefore, difficult to interpret. Data being collected for the Pfizer study cannot accurately be commented on until it undergoes rigorous peer review for publication in a good quality scientific journal.”
Effectiveness of protection
“90% effectiveness sounds surprisingly high. But we have no idea what the demographics look like. Although they opened the trial to high-risk people, we have no idea who contracted COVID-19. As an extreme example, if all the vaccinated volunteers that got COVID-19 were elderly and that number was not significantly different from the elderly among the non-vaccinated volunteers that got COVID-19, that would tell us that the vaccine does not work in those who need it most.
Most of the cases of COVID-19 in the study were presumably mild to moderate since no hospitalizations or deaths were reported, so we don’t know how protective the vaccine will be for those who are susceptible to severe cases.
There is no data regarding immunological memory, which is the entire point of a vaccine. If the memory response is weak or wanes too quickly, people will not be protected over the long term. This would be a fatal flaw because the global roll-out of a vaccine will take a very long time.
Pfizer hasn’t stated what the qualitative nature of the vaccine-induced immune response is. Sub-unit vaccines like theirs have been known to be misinterpreted by the immune system as being an extracellular pathogen. If that is the case, people who receive this vaccine might have a bias imprinted on their immune system that could cause them to respond to natural infections with future coronaviruses in a sub-par fashion.”
Two dose vaccine.
- “It can be hard to get people back for a second dose. It is probably achievable in urban centres but could be hard to get the same people back 21 days later in remote and/or difficult-to-access places, especially in developing countries.
- A vaccine that needs two doses is arguably a ‘weak’ vaccine. For this vaccine, it will take 28 days to build up sufficient protection. So there will be a one-month window during which people will remain susceptible. A better quality, single-dose vaccine could probably reduce this to 10-14 days.
- Fewer than 500 million people could be vaccinated within a year of the vaccine being approved. The company is going to try to stockpile 50 million vaccines this year in anticipation of the vaccine being approved, and they optimistically predict that they can make 1.3 billion doses by the end of 2021. This sounds like a lot, but a two-dose regimen cuts the number of people that can be immunized in half. The person to get the 500 millionth dose will have to wait a year compared to the person who gets the first one. Some will wonder why some people get two doses while they get none. The vaccine won’t be protective unless two doses are given.”
Roll out internationally
“What about the rest of the population? As many of us have been predicting, it could take years to roll out these vaccines. Approval of a vaccine doesn’t help anyone; what matters is when it has been administered and sufficient time has passed for the immune system to respond. Of course, where in this very long timeline for the roll-out will countries that have used strict isolation to control their cases be (arguably, low on the priority list). Pfizer’s press release is essentially saying that everyone beyond the first half-million people will have to wait over 1 year. Presumably, it also means that people beyond the first billion or so may have to wait over 2 years.”
Long term safety
“Long-term safety in people is inferred based on animal models (such as rodents) that have shorter lifespans. Usually, clinical trials are done sequentially and span quite a few years. So acute and some long-term (i.e. 4 or more years) safety data would be in-hand. With the different trial stages overlapping and being run faster than normal, we will likely have less than a year’s-worth of safety data. Ultimately, the only way to be completely sure about long-term (i.e. beyond the duration of the clinical trial phase) safety in people is to monitor vaccinated people for a long period of time after the roll-out. Things like long-term kidney damage, etc. can often (but not always) be predicted/ruled out by things like blood chemistry within the acute stages.”
/ends

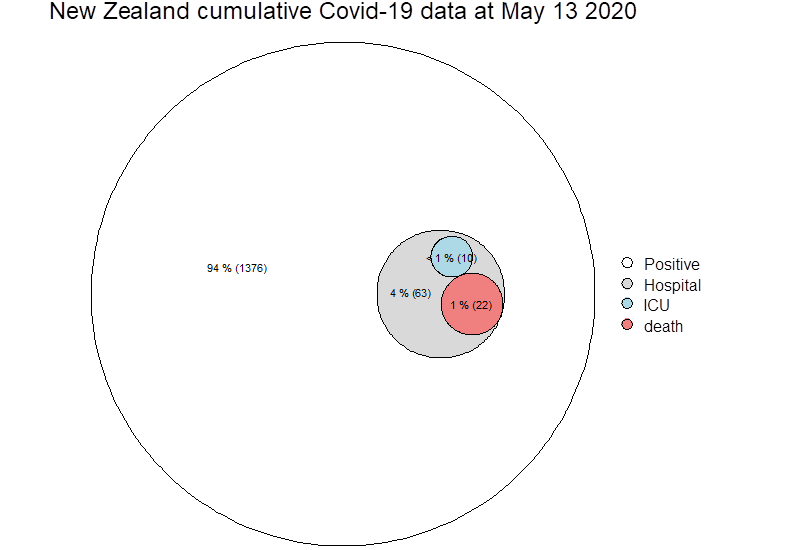
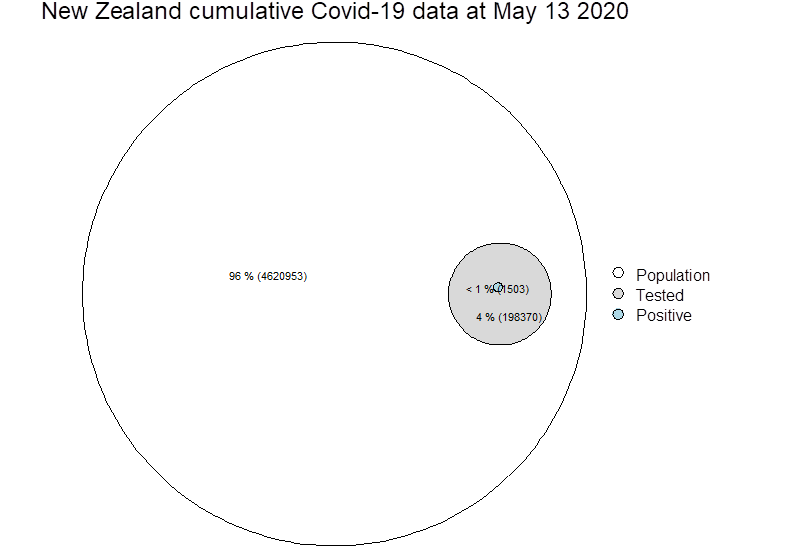 Zeroing on test positive cases (blue circle above, now below), it is not possible from paper to know how many deaths actually went to ICU, so these cells may not be mutually exclusive…
Zeroing on test positive cases (blue circle above, now below), it is not possible from paper to know how many deaths actually went to ICU, so these cells may not be mutually exclusive…