After sparking the first serious debate in New Zealand about the best way of beating Covid-19, Simon Thornley, a member of the Plan B group, explains why he has hope for a safe and swift exit.
There are two approaches offering hope for beating Covid-19.
The Government says the threat is terrible, so elimination is necessary, and that will require a long period of management.
The public health professionals in our group say the threat is major for a small number of people, but we can and must protect them, that the virus wave is abating and immunity growing, and that means we can exit early. Fortunately, that also means hundreds of thousands of people can be saved from economic disaster.
The data shows that internationally and here, the threat of Covid-19 is abating. History will tell us whether this was from lockdown, or immunity growing. That doesn’t matter now, because the data points to the same conclusion: we can shift into what our government calls Level 2.
The major threat is not Covid-19, but the talk of eliminating it and hanging on for a vaccine.
Waiting for a vaccine sounds like soldiers telling each other that their misery will be over by Christmas. But Christmas comes and they are still in the trenches.
As an epidemiologist, I know that vaccines often don’t arrive. I remember the first time I heard that a vaccine for rheumatic fever was five years away. That was ten years ago. There still isn’t one.
Elimination is an impressive goal. We will be the first country in the world to achieve it. But I’m not sure people appreciate what that requires. It is only viable if every person who gets Covid-19 is identified, tested, isolated and quarantined. That’s hard, because at least half of people with Covid-19 don’t know they’ve got it.
I found this out in the recent Auckland measles outbreak. Much of the community were immune, and cases presented in typical fashion. It didn’t end because we stopped it, but because the disease burnt out. People who were susceptible to measles developed immunity, until the disease could no longer spread. For measles, we had additional weapons at our disposal too: we had a reliable test for immunity and a vaccination.
COVID-19 is sneakier than measles. Iceland found out that about half of test-positive cases had no symptoms. Almost 1% of the community tested positive. If the same were true in New Zealand, 50,000 people would now have the virus.
To eliminate the virus we have to find every person and quarantine them to prevent further spread. We’re a small country. We could do it.
But is it worthwhile if population immunity is doing the job? The finding of widespread immunity was an important landmark in the fight against swine flu in 2009. The disease was not as serious as first thought – and immunity was high enough to halt the spread of the virus. A German study showed that in one town, 14% were immune, while 2% had active infection. A similar US study reported that about 3% were immune.
In New Zealand, we don’t know the level of immunity to Covid-19. Perhaps our immunity levels are already high and the virus is being eliminated ‘naturally’. Like swine flu, we need to test for immunity before we take on the Herculean task of eliminating it.
Our hope is that immunity is occurring, because that means New Zealand can exit swiftly. Unfortunately, there are signals that it’s not happening as fast as elsewhere.
Since New Zealand started lockdown, active infections have declined from their peak by 22%, whereas Australia has fallen more steeply (44%).
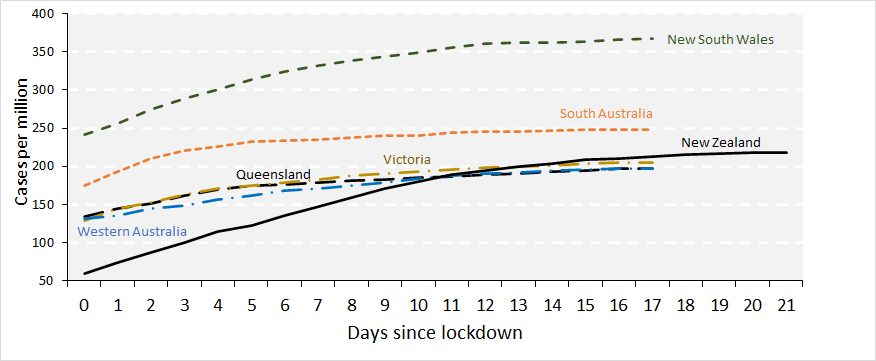
Since the lockdown, cumulative per capita cases have grown at a greater rate in New Zealand compared to most Australian states (Figure 1). Infected cases have progressively declined for the last three weeks in Australia. Australia has had a much looser definition of lockdown, with 90% of the economy continuing to operate, compared to about 50% here.
This is similar to other countries which have soldiered on, albeit with “distance” practices, such as Sweden, Taiwan, Hong Kong, Iceland, and South Korea.
Let’s address again the threat posed by the virus.
In a conservative estimate, Cambridge statistician David Spiegelhalter noticed that age-related mortality rates from the virus in Wuhan closely matched annual mortality rates in the British population.
His conclusion was that getting the virus is like squeezing one year’s mortality risk into two weeks or so – the duration of the illness.
Whether we like it or not, people aged more than 80 years have a one in ten chance of dying each year – that is similar to their chance of dying with COVID-19.
Yes, there have been “thousands of deaths” as the headlines claim – but these are not unexceptional. Overall mortality is indeed high in Europe because Covid-19 does compromise health, but no higher than observed during the 2016/17 influenza season.
This gives hope that, with our lower population density, the virus is not going to overburden our health system – which was one of the main drivers for the lockdown.
The threat of economic disaster scares me personally just as much as the threat of the virus initially scared me professionally. Rising unemployment, business closure and State benefits remind me of my childhood, deeply affected by Dad’s unemployment and consequential mental health.
My hope is that other kids don’t have to experience what I did. The data shows we don’t need to wait until Christmas – we can emerge from our trenches now.
Simon Thornley, Senior Lecturer Epidemiology and Biostatistics, The University of Auckland.
Note: Figure 1. Cumulative cases (PCR positive) of COVID-19 per million, by days since lockdown, comparing New Zealand with Australian states.
Source: Australian and New Zealand Government statistics.