When it comes to Covid19, some scientists and academics are not living up to the expected standards of known facts, free enquiry and open discussion…
Scientists who express different views on Covid-19 should be heard, not demonized
When it comes to Covid19, some scientists and academics are not living up to the expected standards of known facts, free enquiry and open discussion…
Scientists who express different views on Covid-19 should be heard, not demonized
The Covid-19 Science and Policy Symposium was held on 17 August 2020. The event took place as a Zoom webinar, bringing together nine international and national experts to analyse the latest science and New Zealand’s response to the virus.
Watch the presentations here.
–
Dr David Katz, Medical Doctor and Preventative Medicine Specialist, New York.
Dr Jay Bhattacharya, Medical Doctor and Professor of Medicine, Stanford University
Dr Byram Bridle, Viral Immunologist, The University of Guelph.
Prof. Sunetra Gupta, Professor of Theoretical Epidemiology, University of Oxford.
Dr Simon Thornley, Senior Lecturer in Epidemiology at the University of Auckland
Prof Ananish Chaudhuri, Professor of Experimental Economics, The University of Auckland
Dr Grant Morris, Associate Professor of Law, Victoria University of Wellington
Ben smith, PH.D – Data Scientist
Dr Carlo Caduff, Associate Professor of Global Health and Social Medicine, Kings College London.
Group member Gerhard Sundborn tells NewstalkZB why lockdowns cannot be in place long enough to eliminate the virus. He knocks it out of the park.
Simon Thornley
27/07/2020
Most New Zealanders believe now that we are in an exalted position on the Covid road. We are world leaders who have beaten a deadly virus thanks to a tough lockdown. Our only threat now remains from overseas travelers who are quarantined at the border. We are now a Covid-19 free paradise. We can stay this way until a promising vaccine from Oxford comes our way. Surely, this is a matter of holding on for a few more months, and then we can put this whole episode behind us and get on with life.
I would like to believe this story, since my life would be much simpler if I followed the official line. But as an epidemiologist, I’m taught to question and to examine the evidence independently. There are a number of assumptions in this story we have been told. Let’s examine them one by one.
The first is that we are dealing with a deadly virus. Early on in the pandemic, it was possible to believe this, as we had only genetic tests of the virus available. The ratio of people who had died with Covid-19 divided by people who tested positive was 3.4%. This is about seven times the usual estimates of fatality from seasonal influenza (<0.5%).
High fatality rates were projected on a grand scale by modelers. These high rates lead to astronomical predictions of death and destruction which justified severe lockdowns.
Throwing the kitchen sink at such a deadly threat made sense. Just as with swine flu in 2009, however, it was soon found that other evidence, such as antibodies detected in blood, showed a totally different pattern. This occurred in 2009 when antibodies were discovered in about one in four of the New Zealand population. The clamour to eliminate the virus lost its legs.
Early in the epidemic, other researchers overseas were pointing to similar evidence. Professor Mikko Paunio, for example, an epidemiologist from Finland, early in the epidemic showed that 27/1000 blood donors had antibodies to the virus in Copenhagen, Denmark. This proportion extrapolated to over a million Danes having seen and recovered from the virus, compared to many fewer ‘official’ cases. The revised fatality rate was 0.13% – nothing to get excited over.
Now, we even have the Center of Disease Control in the US using 0.65% as a working estimate. This is derived from a summary paper which averaged the results of 26 individual studies. This revised figure is in the scale of severe influenza, and scales down the threat of the virus to just above that of seasonal influenza. These estimates don’t take into account more information about T-cells which now show an even wider exposure to the virus than from antibodies alone. This means that even these revised estimates are very conservative and should be lower still.
In New Zealand, it is clear from looking only at cases, that risk of fatality is higher for older people (Table). People aged over 90 years have not fared well after infection, but conversely, we have now had no deaths from the virus in people aged under 59 years.
Table. Covid-19 cases in New Zealand, by clinical status and age group (at 20 July 2020).
| Age Group (years) | Active | Recovered | Deceased | Case fatality ratio* (%) | Total |
| 0 to 9 | 1 | 37 | 0 | 0 | 38 |
| 10 to 19 | 0 | 122 | 0 | 0 | 122 |
| 20 to 29 | 8 | 365 | 0 | 0 | 373 |
| 30 to 39 | 9 | 239 | 0 | 0 | 248 |
| 40 to 49 | 1 | 221 | 0 | 0 | 222 |
| 50 to 59 | 3 | 247 | 0 | 0 | 250 |
| 60 to 69 | 2 | 177 | 3 | 1.67 | 182 |
| 70 to 79 | 2 | 71 | 7 | 8.97 | 80 |
| 80 to 89 | 0 | 23 | 7 | 23.3 | 30 |
| 90 or more | 0 | 4 | 5 | 55.6 | 9 |
| Total | 26 | 1506 | 22 | 1.44 | 1554 |
*The ratio of deceased PCR test-positive cases divided by the sum of both deceased and recovered. The infection fatality ratio is likely to be much lower owing to serology and T-cells pointing to more widespread infection compared to PCR test-positive cases only. 95% confidence intervals calculated by exact binomial method. CI: confidence interval.
Source: https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-current-situation/covid-19-current-cases Accessed 20 July 2020.
It is also clear that around the world the average age of death of Covid-19 patients is near that of the average life expectancy of that country. This is also clear for New Zealand (figure 1), where the shape of the age distribution of Covid-19 deaths closely approximates the spread of deaths over the same period the year before. A formal test for differences in counts between these data sources shows no evidence of difference. It is very difficult to argue from this plot, that Covid-19 is shortening life spans.
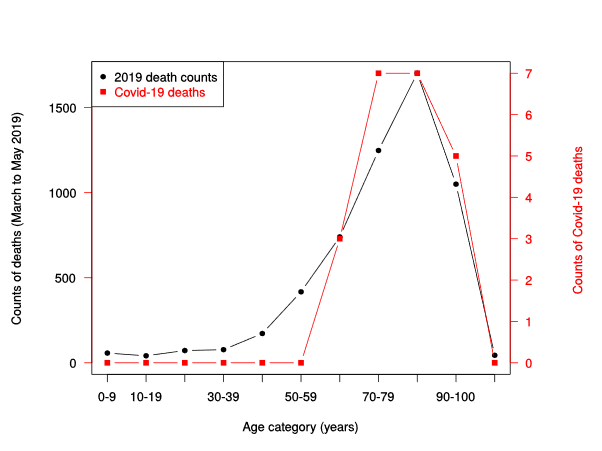
Figure 1. Counts of NZ deaths March to May 2019 (black line), compared to counts of deaths from Covid-19 (red line, right vertical axis), by age category.
Sources: https://fyi.org.nz/request/12583-number-of-deaths-by-age-group-and-week-for-the-last-5-years-dia
https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-current-situation/covid-19-current-cases Accessed 20 July 2020.
Although commentators are lampooning Sweden and their Covid-19 death rates, it is clear that countries with harsh lockdowns, such as Peru have higher rates of Covid-19 deaths than Sweden. Belgium, UK and Spain, all locked down but suffered higher rates of Covid-19 deaths than the comparatively liberal Swedes. Just what explains the difference between these country’s rates of Covid deaths is still unclear, but much is likely to be explained by differences in recording of deaths, demographic differences and population density. We now know that national lockdowns during the epidemic are not associated with an expected reduction in Covid-19 deaths.
Despite the avalanche of evidence coming from overseas, the New Zealand Ministry of Health has clearly stated that it has little interest in serology and is not planning a serosurvey. This strongly indicates that an updating of the fatality of the virus is unlikely in New Zealand, at least in official circles.
Where does this leave New Zealand? Our borders remain closed and both political parties are doubling down on this action. In contrast, other countries including the vast majority of Europe, Iceland, China, and the UK are opening up their borders. Iceland has had its borders largely opened, albeit with virus screening, since June 15 with no evidence of a further outbreak (figure 2). It is clear that these governments have learned from new information, reassessed the risk posed by the virus to their populations, including their immune status.
Evidence of widespread immunity, both in the form of antibodies and T cells is growing. In New Zealand, our politicians and health leaders have little interest in investigating this important issue. A vaccine is simply not a realistic proposition for at least another four years, if not ten. Our tourist economy and borders simply cannot wait this long. We will be held hostage to a story associated with the virus that is well past its “used by” date.
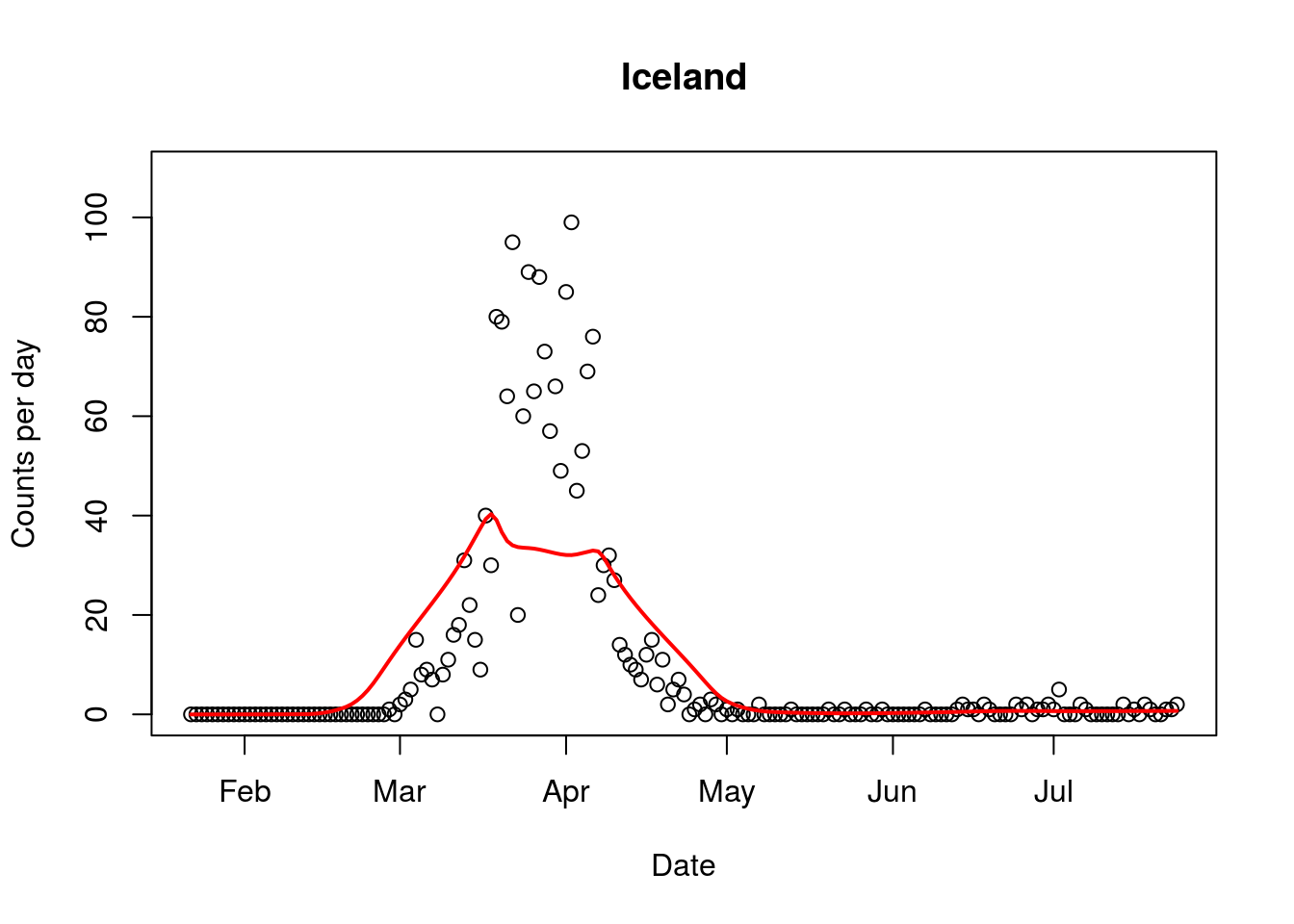
Figure 2. Covid-19 epidemic curve from Iceland, with border opening occurring in mid June. Red line indicates average trend.
In a stunning interview, Professor Carl Heneghan from the Centre for Evidence Based Medicine at Oxford says:
“If you follow the New Zealand policy of suppressing it to zero and locking down the country forever, then you’re going to have a problem… This virus is so out there now, I cannot see a strategy that makes suppression the viable option. The strategy right now should be how we learn to live with this virus.
“The benefits of the current strategy are outweighed by the harms…When it comes to suppression, only the virus will have a determination in that.”
https://unherd.com/thepost/oxford-epidemiologists-suppression-strategy-is-not-viable/
Media Statement
8 July 2020
The Government has formally confirmed that it will not use any of the current or future serology tests to assess how widespread the Covid19 disease has been in New Zealand.
In answer to an Official Information Request by the Covid Plan B group, the Director of the COVID-19 Health System Response team in the Ministry of Health said serology tests would underestimate the true level of exposure to Covid-19.
Epidemiologist Simon Thornley says the new policy is the opposite of what was done in 2009 when serology data on low prevalence of swine flu convinced health officials not to take extreme control measures.
“Serology testing will underestimate the true prevalence, but that will be many times more accurate than just guessing from tests of people presenting with symptoms.
“Fear and uncertainty are driven by lack of information. The more we know, the better we can fight disease. It has been the policy in the past, so it’s strange not to do it now.”
Thornley says a consistent picture is emerging that nose tests for Covid-19 are only picking up a small fraction of all cases.
“Antibodies, present in the blood as well as T cell immune responses to the virus are revealing the coronavirus has reached far more people than listed in the daily “cases” statistic.
“That is important because it would reveal the true effectiveness of our protective measures, and the true state of our population immunity to coronavirus.”
In response to the OIA request for data from serology testing, the Government confirmed:
“Currently there are no Ministry sanctioned seroprevalence studies being performed”.
It claimed that this was supported by a letter in the Nature Medicine journal which indicated that one study found variability in individuals; 40% of asymptomatic people became seronegative and 13% of symptomatic people became negative for IgG [An immunoglobulin] as they recovered.
It noted that a study had been undertaken by the Southern DHB, and that “Positive COVID-19 cases from the Southern DHB study will be confirmed on a second assay to increase positive prediction value.” It said “future studies will have to learn from the Southern DHB study and adapt its methodology accordingly.” The Ministry added that there had been blood mononuclear cell collection by the University of Otago which would be used to perform future mediated response testing.
/ends
Contact Simon Thornley 021 299 1752
Simon Thornley, Gerhard Sundborn
4 July 2020
With a smattering of new cases emerging from returnees in hotels prompting both sides of the house to double down on our tight quarantine the key question is coming into focus: where does our nation go from here?
Sir Peter Gluckman, Rob Fyfe and Helen Clark have recommended starting to reopen our borders. On the other hand, both Dr Ashley Bloomfield and PM Jacinda Ardern have talked about being prepared for further lockdown-like restrictions, with tight border control. Victoria, a state with similar characteristics to New Zealand, has had a recent spike of cases and has decided to enforce local lockdowns, which is a worrying prospect. Which road is best? To open up or to hunker down? Can science help us with this decision?
The latest information on the virus can help us decide which of the Covid-19 roads is best. Its relevance is underlined by the fact it also helps explain why some of the predictions about the fatalities from the virus in New Zealand were 500 to 3,600 times greater than what is happening.
The assumption until now has been that we were all sitting ducks and that we were — and remain — completely at the mercy of the virus. And that assumption underlies the current anxiety about reopening without an effective vaccine to protect us.
The latest science reveals the battle our bodies have had with this virus —and it indicates we are not as defenseless as we might think. Our blood has two major weapons in the fight against viruses: B and T cells, which together are called lymphocytes or pus cells. B cells are like missile factories, making antibodies that lock onto free virus in the body. Most tests to see if anyone has been exposed to the virus look for these antibody B cells.
T cells are more like hitmen who destroy host cells already infected with the virus. T cells are less commonly considered in testing for previous exposure. A feature of Covid-19 is that levels of both these cells (lymphocytes) are unusually low in severe cases most likely because they have been working overtime to fight infection.
A recent study out of the Karolinska Institute in Sweden confirms this idea. A team of researchers tested the blood of 203 people, some of whom had had Covid-19 (by genetic test), looking for evidence that the immune system of these subjects had seen the virus. Among healthy blood donors, who had never tested positive for Covid-19, the researchers found that 4/31 (13%) had antibodies but 9/31 (29%) had positive T cell responses to the virus. That indicates that many more people had been exposed to the virus (and not fallen ill) than indicated by B cell tests alone.
In family members of people with Covid-19, 17/28 (60%) had positive antibodies (B cells), but almost all (26/28; 93%) had positive T cell tests. Almost all genetic test positive cases of Covid-19 had both immune markers. Some may debate the importance of the T cell tests and whether they confer immunity. The researchers are guarded, but indicate that such responses are similar to the immune response of vaccines for other viruses.
What relevance does this knowledge have to us here in New Zealand, considering who to let in and out of the border? As indicated above, it explains why modelling of Covid-19 was so staggeringly inaccurate. Many more of us than we ever knew have microscopic missiles and hitmen in our system on our side. This helps explain why the predicted flood of cases to our intensive care wards and hospitals never eventuated. And this helps us be more realistic about the risk posed by the virus.
What else can we learn from this study? A critical question now is how immune is our population? We have previously summarised the rates of Covid-19 antibodies measured in populations around the world ranges from 0.5 to 26%. The Swedish researchers have shown that the proportion of people in the general population who are likely to be protected from Covid-19 is actually about three times the proportion who have Covid-19 antibodies. This would mean that likely protection from the virus is far more widespread than the antibody surveys indicate. In New Zealand, we are still waiting for any results from antibody tests. The media has reported that tests have been carried out but no data is being made available. Surely the results of this study, even if preliminary, are of critical importance?
So, how does this help us address the border question? If we really want to know what our risk is posed by the virus, we need to take a keen interest in our population’s immune status, as the Swedes have done. The findings of the Covid-19 virus in France and Spain well before the ‘official epidemic’ hit means that many of us have likely encountered the virus before without even knowing it.
Now, in many countries, deaths with the virus are waning, even if in some countries, cases are increasing. The lack of large second waves as Europe is progressively opening up gives us some confidence that immunity to the virus is much more widespread than we initially thought. The debate about our supposed exalted status having ‘eliminated’ the virus is becoming less relevant as evidence accumulates that many of us have already seen the virus, become immune and moved on.
Some commentators have highlighted the paradox of being a Covid-free cul-de-sac. It is our view that we need to adjust to living with the virus and accept that further cases are likely to occur. If our level of natural protection is much higher than thought we need to urgently reconsider whether the elimination strategy, its implications for further lockdown, and an unknowable period of continued border closure, is really worth the financial pain it will continue to inflict. And let’s not forget Covid-19 is not entirely unique. We already accept the risks of living with a number of coronaviruses that have similar characteristics to Covid-19, including: HKU1, 229E, OC43 and NL63.
The implications of this statement by vaccine researchers are profound.
They say that a vaccine for Covid19 won’t be found in time to make a difference to the natural outcome of the pandemic.
So is NZ still planning to wait?
It typically takes a minimum of 10 years for a vaccine to complete the three consecutive phases of the clinical research pipeline. This is because of the scope and length of the experiments, the need to critically assess the results at each stage and the mountains of paperwork that are involved.
We contend that a safe and effective vaccine against severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2), which is the causative agent of coronavirus disease COVID-19, most likely cannot be made available to the public in time to make a substantial difference to the natural outcome of this pandemic. People often cling to hope even when prospects of success are low. However, this can have negative consequences if that hope is not realized.
https://theconversation.com/fast-covid-19-vaccine-timelines-are-unrealistic-and-put-the-integrity-of-scientists-at-risk-139824
https://www.orlandomedicalnews.com/article/3545/letter-to-the-editor-why-increasing-number-of-cases-of-covid-19-is-not-bad-news
By JOHN T. LITTELL, MD
Several times a day, on every possible news outlet, we are bombarded with updates as to the new number of “cases” of COVID-19 in the U.S. and elsewhere. News analysts then use these numbers to justify criticisms of those who dare to reject the CDC’s recommendations with regards to mask wearing and social distancing. It is imperative that all Americans – and especially those in the medical profession – understand the actual definition of a “case” of COVID -19 so as to make informed decisions as to how to live our lives.
Older Americans remember all too well the dread they experienced when a family member was diagnosed with a “case” of scarlet fever, diphtheria, whooping cough (pertussis), or polio. During my career in family medicine, including several years as an Army physician, I have cared for patients with chickenpox, shingles, Lyme disease as well as measles, tuberculosis, malaria, and AIDS. The “case definition” established for all of these diseases by the CDC requires the presence of signs and symptoms of that disease. In other words, each case involved a SICK patient. Laboratory studies may be performed to “confirm” a diagnosis, but are not sufficient in the absence of clinical symptoms.
Having now been privileged to care for sick patients with COVID-19, both in and out of the hospital setting, I am happy to see the number of these sick patients dwindle almost to zero in my community – while the “case numbers” for COVID-19 continue to go up. Why is that?
In marked contrast to measles, shingles, and other infectious disease, “cases” of COVID-19 do NOT require the presence of ANY symptoms whatsoever. Health departments are encouraging everyone and anyone to come in for testing, and each positive test is reported as yet another “new” case of COVID-19!
On April 5, 2020, a small number of state epidemiologists (Council of State and Territorial Epidemiologists (CSTE) Technical Supplement: Interim-20-ID-01) came up with a “surveillance” case definition for COVID-19. At the time, there was uncertainty as to whether or not completely asymptomatic persons could transmit COVID-19 sufficiently enough to infect and cause disease in others. (This notion has never been proven and, in fact, has recently been discounted – cfr “ A Study on the Infectivity of Asymptomatic SARS-CoV-2 Carriers, Ming Fao et al, Respir Med, 2020 Aug – available online through PubMed 2020 May 13, as well as recent reports from the WHO itself). The CSTF thereby justified the unconventional case definition for COVID-19, adding “CSTE realizes that field investigations will involve evaluations of persons with no symptoms and these individuals will need to be counted as cases.”
Hence, anyone who has a positive PCR test (the nasal swab, PCR test for COVID Antigen or Nucleic Acid) or serological test (blood test for antibodies –IgG and/or IgM) would be classified as a “case” – even in the absence of symptoms. In our hospitals at this time, there are hundreds of former nursing home residents sitting in “COVID” units who are in their usual state of good health, banned from returning to their former nursing home residences simply because they have TESTED Positive for COVID-19 during mass testing programs in the nursing homes.
The presence of a positive lab test for COVID-19 in a person who has never been sick is actually GOOD news for that person and for the rest of us. The positive test indicates that this person has likely mounted an adequate immune response to a small dose of COVID-19 to whom he or she was exposed – naturally (hence, no need for a vaccine vs. COVID-19).
It is important as well to understand that the presence of lab testing is not the ONLY criterion that the the CDC uses to established a diagnosis of COVID-19. The presence of only 1 or 2 flu-like symptoms (fever,chills, cough, sore throat, shortness of breath) – in the absence of another proven cause (e.g., influenza, bacterial pneumonia) is SUFFICIENT to give a diagnosis of COVID-19 – as long as the patient also meets certain “epidemiological linkage” criteria as follows:
“In a person with clinically compatible symptoms, [a “case” will be reported if that person had] one or more of the following exposures in the 14 days before onset of symptoms: travel to or residence in an area with sustained, ongoing community transmission of SARS-CoV-2; close contact (10 minutes or longer, within a 6 foot distance) with a person diagnosed with COVID-19; or member of a risk cohort as defined by public health authorities during an outbreak.” Note that the definition of a “risk cohort” includes age > 70 or living in a nursing home or similar facility.
So, in essence, any person with an influenza- like illness (ILI) could be considered a “case” of COVID-19, even WITHOUT confirmatory lab testing. The CDC has even advised to consider any deaths from pneumonia or ILI as “Covid-related” deaths – unless the physician or medical examiner establishes another infectious agent as the cause of illness.
Now perhaps you see why the increasing number of cases, and even deaths, due to COVID-19 is fraught with misinterpretation and is NOT in any way a measure of the ACTUAL morbidity and mortality FROM COVID-19. My patients who insist upon wearing masks, gloves and social distancing are citing these misleading statistics as justification for their decisions (and, of course, that they are following the “CDC guidelines”). I simply advise them, “COVID-19 is NOT in the atmosphere around us; it resides in the respiratory tracts of infected individuals and can only be transmitted to others by sick, infected persons after prolonged contact with others”.
So you may ask – why are we continuing to report increasing numbers of cases of COVID as though it were BAD news for America? Rather than as GOOD news, i.e, that the thousands of healthy Americans testing positive (also known as “asymptomatic”) are indicative of the presence of herd immunity – protecting themselves and many of us from potential future assaults by variants of COVID?
Why did we as a society stop sending our children to schools and camps and sports activities? Why did we stop going to work and church and public parks and beaches? Why did we insist that healthy persons “stay at home” – rather than observing the evidence-based, medically prudent method of identifying those who were sick and isolating them from the rest of the population – advising the sick to “stay at home” and allowing the rest of society to function normally? And, while we witnessed the gatherings of protestors in recent days with little concerns for COVID-19 spread among these asymptomatic persons, most certainly many are hoping that the increasing “case” numbers for COVID-19 will discourage folks from coming to any more rallies for certain candidates for political office.
Fear is a powerful weapon. FDR famously broadcast to Americans in 1933 that “We have nothing to fear, but fear itself”. I would argue that we have to fear those who would have us remain fearful and servile and willing to surrender basic freedoms without justification.
John Thomas Littell, MD, is a board-certified family physician. After earning his MD from George Washington University, he served in the US Army, receiving the Meritorious Service Medal for his work in quality improvement, and also served with the National Health Service Corps in Montana. During his eighteen years in Kissimmee, FL, Dr Littell has served on the faculty of the UCF School of Medicine, President of the County Medical Society, and Chief of Staff at the Florida Hospital. He currently resides with his wife, Kathleen, and family in Ocala, Florida, where he remains very active as a family physician with practices both in Kissimmee and Ocala. To learn more, visit johnlittellmd.com
Around the world, governments that had appeared to tame the coronavirus are adjusting to the reality that the disease is here to stay. But in a shift away from damaging nationwide lockdowns, they are looking for targeted ways to find and stop outbreaks before they become third or fourth waves.
https://www.nytimes.com/2020/06/24/world/europe/countries-reopening-coronavirus.html