14/09/2021
Many areas of the world are now in a race to achieve high coverage of covid-19 vaccination. Some commentators in New Zealand are now criticising the government for not rolling out fast enough. Given the high efficacy of many vaccines, this seems like a sensible strategy, but is it?
The government recently asked some of New Zealand’s epidemiology experts “Is an elimination strategy still viable as international travel resumes or are we going to need to accept a higher level of risk and more incidence of COVID in the community”. The specialists concluded that: “There is no doubt that this strategy has served us well”, comparing deaths in New Zealand attributed to covid-19 of 26 to 10,000 in Scotland. The way out was through high levels of vaccination. The document assumes that elimination is the ‘optimal’ strategy and further incursions, we are assured, will be ‘stamped out’ as we achieve high levels of vaccine induced immunity.
Will this really eventuate? In terms of rapid vaccine rollouts, Iceland is a counter example. Icelanders have now vaccinated 69 or 81% of their population, depending on whether you consider the whole population or only those eligible for vaccination (12 years and over). Almost all Iceland’s older generations are now vaccinated (99% coverage of 70 to 79 years), yet the younger generation has slightly lower coverage (78% of 30 to 39 years). However, the vaccination records of covid-19 cases there tells another story: 73% of cases are fully vaccinated. This figure is inconsistent with the trial evidence of efficacy of the vaccine being 95% in reducing symptomatic infections (95% confidence interval: 90.3 to 97.6%). If this efficacy were correct, covid cases would be expected to only yield a small fraction of people with records of full-immunisation [(69% – 95% * 69%)/(1 – 69% * 95%) = 10%]. As almost three-quarters (73%) of recent cases in Iceland are fully vaccinated the efficacy obtained in the trial does not match the reality of the roll-out.
Others are noticing similar results: a recent case-series in the US also showed 74% of cases were vaccinated, with PCR cycle threshold values, roughly assumed to be equivalent to infectivity, similar in vaccinated and unvaccinated cases.
A case is being made for continuing vaccination since deaths may be prevented in those vaccinated. However, in the UK, a Public Health England recent report shows that of all dominant delta variant cases occurring from 2 February to 3 August 2021 (n = 300,010), 15.7% (47,008/300,010) were fully vaccinated compared to 50.3% (151,054/300,010) unvaccinated. The remainder were either partially vaccinated or their status was unknown. A total of 741 deaths occurred in the delta cohort (0.25%; 741/300,010) within 28 days of testing PCR positive, with 90% of deaths (670/741) occurring in those aged over 50 years (figure; five unlinked cases are removed). The outer grey square represents the total cohort who tested positive for delta variant, with the blue rectangle the cases aged less than 50 years, the beige those who had been fully vaccinated, the dark green those who were hospitalised and the light green the deaths. One can immediately appreciate that deaths are few in the delta cohort and that most people do not need hospital treatment, even in the over 50 age group. This means that delta is hardly the “game changer” the Prime Minister has talked of.
Analysis of the delta cohort points to differential associations between exposure to the vaccine and death within a month. When the cohort is divided by age, deaths associated with covid-19 are 1.57 times (95% confidence interval (CI): 0.85 to 2.89, not significant) more likely in the vaccinated group under 50 years, compared to unvaccinated, whereas in the older bracket the vaccinated are 70% less likely to die from covid-19 compared to the unvaccinated (95% CI: 84 to 64%). The vaccine’s ability to prevent covid-19 deaths in younger age groups among people with the delta variant is certainly questionable from these data. It must also be remembered that these calculations are crude in the sense that they do not account for comorbid status of delta ‘cases’.
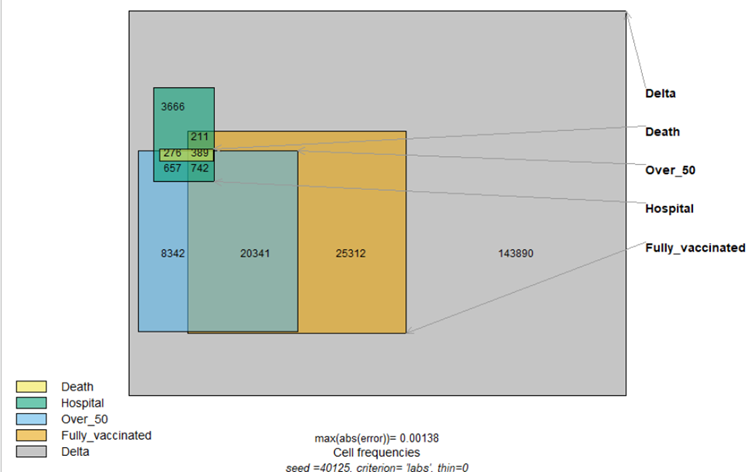
Figure. Scaled rectangle diagram, illustrating the fatality proportion of the UK delta variant case cohort, by vaccination status, age and need for hospital care. Some counts of small cell values and those with uncertain vaccination status (n = 31,841) have been omitted. This includes 13 deaths occurring in the ‘fully vaccinated’ under 50 years, 56 in the ‘unvaccinated’ group under 50 and 7 were unlinked, making 741 total deaths.
The best evidence of overall effect on death comes from the latest update of the Pfizer trial which shows slightly more overall deaths (15/21,926) occurred in the vaccinated group than in controls (14/21,921). This is important, since the outcome doesn’t just count successes (reduced covid ‘cases’), but also includes the possibility of vaccine harm, evaluating the effect of the vaccine on overall survival. This means the best evidence thus far indicates a 7% increase in risk of death, comparing the vaccinated to the unvaccinated. Yes, the numbers are small, and these results are compatible with a wide range of vaccine effects, but it seems strange that this important information is relegated to the study appendices and is absent from the summary. Most of us are more interested in our overall longevity, rather than being solely focused on avoiding covid-19. The Prime Minister’s claim (52’:27”) that the vaccine is “saving lives” is sounding hollow, from the best possible epidemiological evidence: Pfizer’s own trial.
The policy response to the recent surge in cases in Iceland is to extend vaccination to pregnant women and impose further restrictions. The UK, in contrast, is dropping restrictions, despite a recent spike in overall case-numbers. As New Zealand is once again thrown into costly lockdowns, we need to ask whether it is appropriate, given the evidence.
We now have a group of scientists advising the government that cannot see any other strategy apart from elimination as ‘viable’ or ‘optimal’. This is understandable, as they have committed the country to this course of action, one that has cost us at least NZ$50 billion. We must now recognize that other courses of action are viable. Sweden, Florida, and Texas demonstrate this. Analysis of excess mortality in Sweden for 2020 has shown a 3 to 8% increase from background which are attributable to past mild influenza seasons. The rush to vaccinate must now be balanced by the questionable efficacy of vaccines demonstrated in Iceland, the accumulating evidence of vaccine-related adverse effects, including the 350 serious reactions on government websites. The enthusiasm for more lockdowns must also be questioned, given evidence of business closures, queues at food banks and the extra 43,000 kiwis on jobseeker support since March 2020.
As we said from early 2020, the path forward lies not in a medical intervention, but rather in a realistic assessment of the threat posed by the virus, based on such evidence as the distribution of age of death with covid-19 being similar to background mortality. Our efforts should be best focused on protecting the most vulnerable, implementing early treatment protocols, increasing capacity in our hospitals, while the majority of those of working age and younger people return to normal life. Overseas data clearly now show that vaccines are not a way out.
